Deep inside the maze of hallways at a research laboratory outside Washington, DC, at the end of a long corridor, is a small window built into the wall.
It provides the only outside view of a dangerous mission: researchers handling samples of the deadly Ebola virus and working with drugs to mitigate it. At biosafety level 4 (BSL4), the lab is at the highest level of danger.
Inside, Spencer Stonier, a virologist, wears a white biohazard or “space” suit. A thick yellow spiral cord is attached to the back. It twirls up to the lab’s ceiling, supplying him with filtered air and puffing out his suit.
Stonier’s heavily gloved hands slowly and carefully work with samples of Ebola in small dishes. His boss, John Dye, says he worries about the danger that his team of scientists expose themselves to in the course of their research.
“I wake up in cold sweat,” said Dye, a viral immunologist leading a team of cutting edge scientists racing to find a drug or vaccine to stem the longest and deadliest Ebola outbreak in history.
VOA was recently granted access to the "hot" labs at Fort Detrick in Frederick, Maryland, one of the famed high security laboratories of the U.S. Army Medical Research Institute of Infectious Diseases (USAMRIID), which handles the world’s most lethal pathogens.
Far from the African villages and cities ravaged by Ebola, researchers are working round-the-clock to halt the current epidemic and prevent future outbreaks of Ebola and similar diseases.
In one capacity or another, Dye, an affable and helpful professional, has been working on a vaccine for Ebola and its cousin in the family of filoviruses, Marburg, at USAMRIID since 2003.
During VOA's visit, Dye at times appeared somewhat nervous, perhaps with exhaustion as he and about 100 scientists, veterinarians and support staff have worked doggedly since the virus began spreading out of control in Guinea, Sierra Leone and Liberia last year.
With a fatality rate between 60 to 90 percent, Ebola is considered one of the most lethal viral infections known to man. The pathogen races through the cells of an infected human, replicating itself quickly while simultaneously dealing a strong blow to a patient’s immune system.
Ebola sufferers become extremely dehydrated due to uncontrollable vomiting and diarrhea and, in the end stages of the disease, they suffer internal and external bleeding.
Dangerous work
Scientists who work in BSL4 labs – USAMRIID scientists call them suites – handling Ebola must go through extensive training before donning protective anti-contamination suits and conducting experiments.
Suiting up is anything but simple. It’s a lesson in step-by-step safety protocols.
It all begins with the hands, said Dave Harbourt, a biosafety officer at USAMRIID, as he taped two pairs of elastic gloves to the end of his long-sleeved undershirt.
“By far, one of the most important checks that you have to do is you have to check your gloves, every time,” he said. “Because whether you’re in BL1 or BL4, your highest area of contamination is always going to be your hands and wrists.”
Wearing the cumbersome suit is exhausting and isolating. Dye won’t let any of his team members work longer than four hours in one.
"It gets very dark, your visor fogs up, it's very cumbersome, it dehydrates you,” Harbourt said. There’s “muscle weakness, fatigue. You're carrying – with air in there – about 40 extra pounds. One of the biggest factors in this work is that it is very time consuming."
Each and every movement requires intense concentration. The simple act of opening a jar or bottle with heavily gloved hands requires slow, deliberate movements to guard against an accident that might lead to exposure.
Once sealed inside a suit, there are no bathroom breaks and there is no conversation.
"You get good at reading lips,” Harbourt said. To communicate, scientists also use hand signals or write on a whiteboard with a pen.
On the day two VOA journalists visited USAMRIID, Harbourt said he did some minor work - changing out some filters - related to an Ebola study in a BSL4 lab.
"If I'm doing that in a lab with this situation, the absence of the suit, it probably takes me 10 minutes,” he said. “It took me an hour and a half to do that this morning."
Despite daily work with the world’s most fatal pathogens, USAMRIID says there have been no lab-acquired infections for researchers working in BSL4 labs. Around 20 so-called “close calls” – needle sticks, a bite or scratch from an animal used in a study, gloves that fail – have been reported.
From bio ‘offense’ to bio ‘defense’
USAMRIID was launched in 1969. when then President Richard Nixon announced the United States would no longer develop deadly biological weapons, something the U.S. government had engaged in since at least World War II.
Driven by perceived threats from Germany and Japan, the United States began an offensive biological program in 1943. For decades, U.S. scientists working at the specialized facility at Fort Detrick weaponized several deadly agents, including anthrax.
But since 1969, the mission at USAMRIID has been to protect United States military personnel and develop vaccines and treatment for the world’s deadliest bugs. Among them: anthrax, tularemia, Q fever, Marburg, Lassa, botulinum toxin and, of course, Ebola, which, according to the latest WHO figures, has killed over 8,800 people and infected another 22,000 so far. Their work is performed on annual budget of about $140 million.
USAMRIID’s approach to Ebola is three-pronged: therapeutic medicine, faster diagnostic tools and, the best answer to controlling Ebola outbreaks, a vaccine. Not long after the World Health Organization and the U.S. Centers for Disease Control and Prevention reported “that this virus was starting to spin out of control … we really stepped up our research here," Dye said.
That means roughly one-third of USAMRIID’s 300 staff scientists are now entirely devoted to Ebola research. That Ebola has engulfed three West African nations weighs heavily on the scientists here.
“We are under tremendous pressure,” said Travis Warren, principal investigator at USAMRIID. “My activities have focused almost exclusively on developing and evaluating anti-Ebola virus therapeutics since approximately June.”
The search for safe and effective drug therapies to treat the infected requires intimate knowledge of how the Ebola virus works.
And scientists must also come up with ways to outsmart the virus: block its ability to infect human cells after exposure, or curtail its rapid replication once inside a cell.
Despite how vicious this particular pathogen is in humans, the Ebola virus is only a single strand of genetic material, containing instructions for just seven proteins.
The virus encodes those instructions on RNA, a chemical cousin of DNA that makes up our genes. Once inside a cell, the virus copies its genes into proteins that, in turn, rapidly assemble copies of the virus.
One cutting-edge approach in the hunt for Ebola drugs is focusing on the virus' RNA, Warren said.
“With an RNA virus, we can…target the viral RNA for destruction in a very specific fashion,” he said. “Once that viral RNA is destroyed, the virus cannot reproduce its own genetic material…then the infection is effectively suppressed.”
USAMRIID and Canadian pharmaceutical company Tekmira helped develop one promising RNA drug called TKM-Ebola. The drug contains a small piece of the virus’s RNA, wrapped up in a package that alerts the cell’s defenses, Warren said.
“There are enzymes that literally chop up the viral RNA and destroy it. Once the viral RNA is destroyed...the virus ceases to function,” he said.
Another trial drug, ZMapp, is based on the proteins our immune systems use to fight infections, known as antibodies.
“We’ve taken a cocktail of three of these antibodies…that are known to fight the virus, and put them all together,” Dye said. “And then we inject that, and that helps to control the virus.”
But a key ingredient of the cocktail comes from tobacco plants and can’t be manufactured quickly. And the last supplies were delivered to Liberia in August.
A third drug, Favipiravir, takes a different path.
Originally designed by Japanese researchers for influenza, the drug is a nucleoside analogue — a molecule that looks like a building block of genetic material. It works by jamming up the machinery the virus uses to copy its genes.
It has shown promise fighting Ebola in animal studies. It is also being tested in Guinea, where the humanitarian group Doctors Without Borders is conducting a clinical trial on humans.
Diagnostics
Of the many complicating factors driving the current epidemic, one of the biggest is figuring out quickly who is sick with Ebola and who isn’t. Currently, people suspected of infection must be monitored for 21 days, the maximum period of incubation.
“Diagnostics are the way we're going to get this Ebola outbreak under control," said USAMRIID virologist Randy Schoepp.
Ebola experts say that accurately determining who is infected plays a key role in contract tracing – another crucial step in stemming an outbreak.
At the moment, a test known as real-time PCR – short for polymerase chain reaction – is being used in the field. The Federal Drug Administration approved it under emergency authorization rules.
“It's a test in which we amplify genomic material and then look for specific signatures,” said Schoepp, who is chief of USAMRIID’s Applied Diagnostics Branch. “It's exquisitely sensitive. And exquisitely specific.”
But real-time PCRs are problematic, especially during a dangerous outbreak. First and foremost, getting a single result takes four hours. And testing is very difficult to conduct at bedside, the most ideal situation during an outbreak.
The diagnostic machine, about the size of a portable television, must be connected to a computer. And Scheopp said it requires a fully functioning lab – another difficulty working in the field presents.
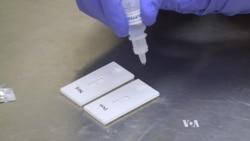
But Scheopp, who went to Liberia earlier in the epidemic, has been working on a possible solution: a plastic stick test that resembles a pregnancy test.
“You can put a few drops of blood on, or in our case it's plasma, you put a few drops of plasma on, allow it to wick through this and if you have Ebola there, it gives you a line. If there is no Ebola there, there is no line."
It’s simple and the results are fast – as fast as 15 minutes. And it can be used at bedside.
“But it has its limitations,” Scheopp said. “For that convenience and quick 15 minute assay, you trade off sensitivity.”
That means health workers need to confirm the results, particularly a negative result, with a real-time PCR machine. But when Scheopp was in Liberia early in the epidemic, he said, there was a lot of confusion among health experts there.
“Even the medical community in Liberia didn’t understand that…our tests were not infallible,” he said.
Still, Scheopp thinks the stick test can best be used in triage situations, contract tracing and handling corpses, which are highly infectious.
Scheopp’s work in Africa during the epidemic this outbreak profoundly demonstrated the importance of a fast, reliable test.
“In Liberia ... that’s when it was all brought home to me because, suddenly, I was making decisions that affected a person’s life,” he said. “It was quite sobering. Kept me up at night."
Trials on the plastic stick diagnostic are currently underway in Liberia. If all goes well, USAMRIID's best guess is that a reliable and portable test may be available in a few months.
Vaccine models
While drugs to help those suffering the ravages of Ebola are a priority at USAMRIID, preventing a future outbreak hinges on finding a safe and effective vaccine.
According to Dye, there are at least a half a dozen vaccines developed and tested at USAMRIID that show 100 percent efficacy in monkeys. In two candidates, USAMRIID researchers have employed the novel approach of using the vector – the genetic material – of the virus to induce an immune response.
“They’re actually taking the genetic material that makes that protein [of the virus], putting that genetic material into the human to make that [viral] protein naturally,” Dye said. “If you put the DNA or RNA in, the genetic material, there’s less chance for it to break down.”
In essence, the method of prompting the body to make the viral protein naturally helps improve the recognition of the virus by the immune system and generate a protective response.
If all goes well, Dye predicts that by early spring there might be a vaccine that could be given to health care workers – those most likely to become infected in West Africa.
Because USAMRIID is part of the Defense Department, its mission also includes another very important objective: that is, anticipating and fending possible bioterrorist attacks. That's why researchers, in addition to protecting the military and public, are driven to get a grip on this disease.
“The CDC and the U.S. government have determined that Ebola is a category A pathogen, which is high-tiered pathogen in that it could be used for intentional release,” Dye said.
The harsh reality is that it will take years to be absolutely certain that an Ebola vaccine actually works. And that bumps up against another reality that plagues Dye.
“What keeps me up at night is the concept [that] as the world globalizes and we are infringing on new habitats of new species of animals, like is going on in Africa, the chances of emerging infectious diseases increases, and I think we’re going to see more infections,” he said.
“Not Ebola per se,” he said. “But like Ebola that we’re going to learn to have to deal with.”
VOA'S Steve Baragona contributed to this report.